SEIU Local 2015 mandatory Covid-19 vaccine principles
On August 5, 2021, when the Governor mandated that all healthcare workers in California be vaccinated, SEIU 2015 members led the way. In anticipation of vaccine mandates, member leaders in nursing homes across the state convened to develop a set of principles to guide continued vaccine rollout.
We spent the past 18 months on the front lines of the COVID-19 pandemic. We saw the ravages up close in nursing homes and private homes up and down the state. We’ve been at the forefront of promoting vaccination in the fight against COVID-19 since it first became available—to protect their vulnerable clients as well as themselves and their families.
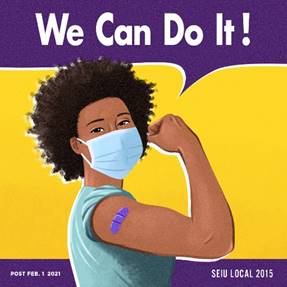
“Through our ‘We Can Do It!’ campaign, we’ve helped tens of thousands of our long-term care providers, their families, and their vulnerable clients access vaccinations across the state,” said SEIU Local 2015 President April Verrett. “We believe vaccination is the best weapon available in the battle against this pandemic, protecting against infection and slowing the development of dangerous variants. Our members are determined to be part of reining in this devastating disease. Together, we will defeat COVID-19.”
“Last year at the beginning of the pandemic, the nursing home where I work was hit hard,” said Christina Lockyer, a Nurse Assistant in Bakersfield. “More than 100 of my co-workers got it. We weren’t provided the proper PPE. It was so bad that the state had to send EMTs to come work here. We lost 19 of our patients to COVID. I’m proud that our Union is leading the way to encourage vaccination. We’re caring for sick people and we need to do everything we can to protect them. That’s why I was part of the working group that developed guidance we want our employers to follow. I want any of my co-workers who might still be on the fence about vaccination to know that they’ll be supported.”
SEIU 2015 members’ recommended principles include:
- There should be vaccination stipends or pay for all vaccinated, including those already vaccinated.
- Employers must make vaccines accessible to all workers, either at or near the workplace
- Vaccinations must be provided on paid time
- Any lost time due to the impact or side effects of vaccinations must be on paid time, including support for any medical follow-up needed.
- Workers must be allowed a reasonable time period to become vaccinated.
- Accommodation must be made for those who cannot get vaccinated, whether due to health or religious reasons.
- Any vaccine mandate must take into account staffing shortages and any impact on staffing.
- Any mandate must include an educational component.
- Vaccinations are NOT a replacement for responsible management, including but not limited to:
- Provision of sufficient and proper PPE
- Regular and Ongoing Training and Communications
- Proper procedures to prevent outbreak
- Isolation to prevent outbreak.
Helpful Links
California Covid-19 Information Website
CA Dept. of Public Health: COVID-19 Vaccine Eligibility for People with High-Risk Medical Conditions or Disabilities
CA Dept. of Public Health: Vaccines for People with High-Risk Medical Conditions or Disabilities
Covid-19 Vaccine Safety and Effectiveness FAQs
Download in your preferred language:
հայերեն | 中文 | English | Hmong | 한국어 | русский | Español | Tiếng Việt